Is it ever okay for a clinician to lie to a patient?
- June 5, 2023
- 0 Likes
- 357 Views
- 0 Comments
APP Colleague’s last post described a scenario:
An elderly patient comes into the dermatology office requesting a prescription refill to treat the “shingles” recurring on their buttocks several times a year. Upon further questioning, it was discovered that the patient’s PCP provided the “shingles” diagnosis to the patient. The dermatology specialist is happy to refill the antiviral medication, but wonders if they should inform the elderly patient that they actually have the sexually-transmitted herpes simplex virus (HSV) – not shingles.
Dr. Sandeep Jauhar equates withholding medical information from a patient as a form of paternalism, and he discusses paternalism’s fading role in medicine in his article “When Doctors Need to Lie.[1]” Dr. Jauhar argues that patients have the right to be fully informed about their conditions and that withholding of information can destroy the clinician-patient relationship. When providing a medical diagnosis, a well-meaning APP may want to prevent the patient from regretting past decisions. Still, some argue that regret can lead to the patient’s personal growth [1]. However, the article argues paternalism still has a role in medicine. Dr. Jauhar describes several scenarios he has faced as a cardiologist in which he had to take such an approach. He concludes that clinicians should keep paternalistic actions on behalf of their patients as “soft” as possible, using negotiation to guide a patient to share the clinician’s perspective [1].
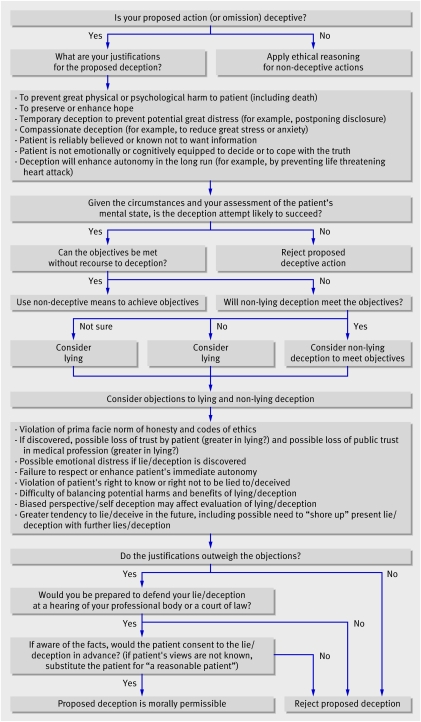
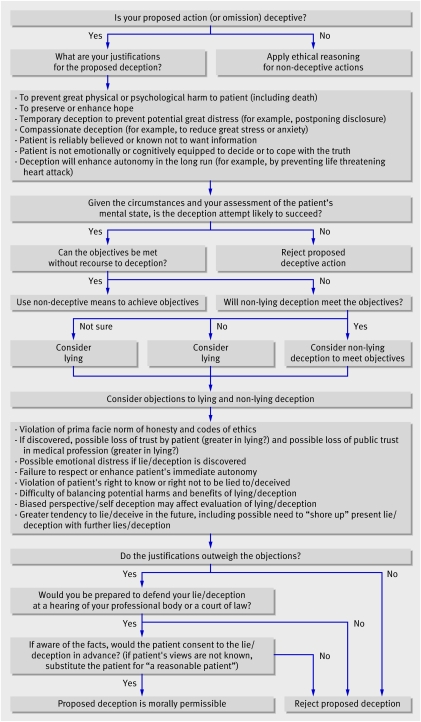
Dr. Daniel Sokol, an expert in clinical ethics, has gone a step further and developed a flowchart to help the “ethically sensitive” clinician make an informed decision (see image on left) [2]. Dr. Sokol believes there are situations where it is morally acceptable to “benignly deceive” patients.
This takes us back to our dermatology scenario… do we inform the elderly patient that they actually have sexually transmitted HSV before prescribing them more antivirals, or do we issue the refill and let the patient continue to believe they have “recurrent shingles?”
When faced with this situation in the clinic, I typically take an approach where I tell the patient I am happy to refill their antivirals, but I want them to understand that their eruption is more like a “cold sore.” It’s viral and contagious, tends to recur in the same location, and is usually acquired earlier in life. I don’t want to cause anyone unnecessary upset, but I want to be honest. I don’t want to disrupt the relationship the patient has with their PCP, but I think people should have an understanding of the condition they are being treated for.
Do you run into a repetitive situation where you aren’t sure how honest to be with a patient? How have you handled it? Looking back, are there any things that you would have handled differently? Please share with your APP Colleagues!
-Nikki Rataj Casady, DMSc, PA-C
References
- Jauhar S. When doctors need to lie. The New York Times. Published February 22, 2014. Accessed May 30, 2023. https://www.nytimes.com/2014/02/23/opinion/sunday/when-doctors-need-to-lie.html
- Sokol DK. Can deceiving patients be morally acceptable? BMJ. 2007;334(7601):984-986. doi:10.1136/bmj.39184.419826.80